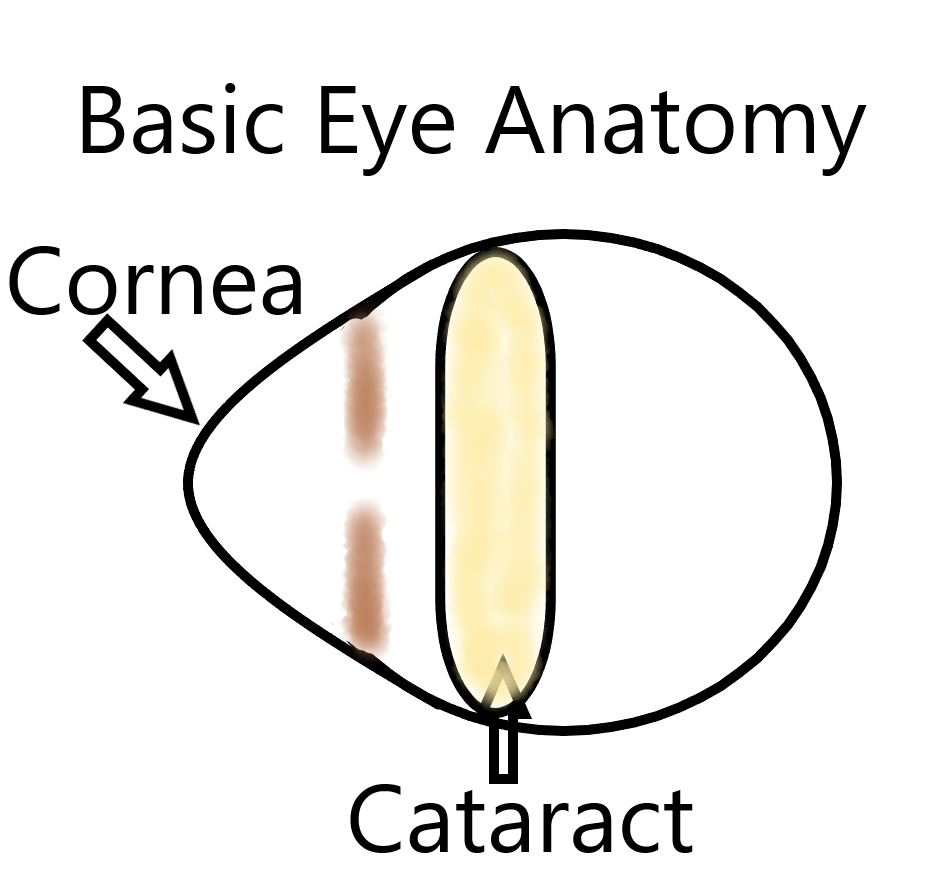
What is a cataract?
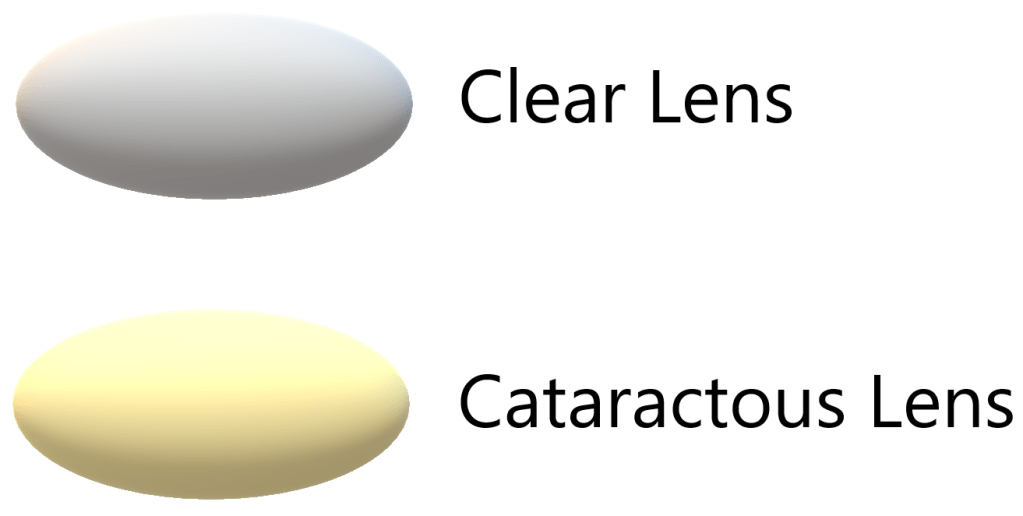
Simply put, a cataract is when the natural lens inside your eye that opacifies over time, ultimately blocking light from passing through your eye to your brain. This happens naturally with aging as proteins break down.
What are the risk factors for getting a cataract?
Age is the most common risk factor. Other factors to consider include trauma, steroid usage, and diabetes (all of which can cause cataracts to occur at a younger age). Cataracts typically become detectable by your eye doctor in your later 40s or early 50s. Your vision is typically not affected until your 60s or 70s.
Are there different kinds of cataracts? Are they treated differently?
There are 3 main types of cataracts:
- Nuclear Sclerotic
- Cortical Spoking
- Posterior Subcapsular
They are all treated with cataract surgery when they begin to affect your vision and ability to function on a daily basis.
Will my cataract get worse over time?
Cataracts do tend to progress over time. Sometimes the cataract progresses very slowly (more typical of a nuclear sclerotic cataract) while other cataracts lead to more rapid deterioration of vision (e.g., posterior subcapsular cataract). Progression can take months to years to decades.
Am I ready for cataract surgery yet?
Cataract surgery is almost always an elective surgery. Rather, the patient needs to tell the eye surgeon when there ability to function on a daily basis is being affected by decreasing vision. If the eye surgeon determines the decrease in vision is caused by the cataract then the patient is ready to undergo this procedure. The threshold for patients can certainly be met when the vision in either eye becomes worse than 20/40 (what a normal person sees at 40 feet you can only see at 20 feet) because of the cataract. Another common complaint cataract patients often have is difficulty with night driving due to glare.
*** If a patient only has 1 eye with good visual potential (i.e., only 1 healthy eye), the threshold to do cataract surgery may be increased to mitigate any risk of damaging the patient’s only good eye.
Can I get cataract surgery to eliminate my glasses?
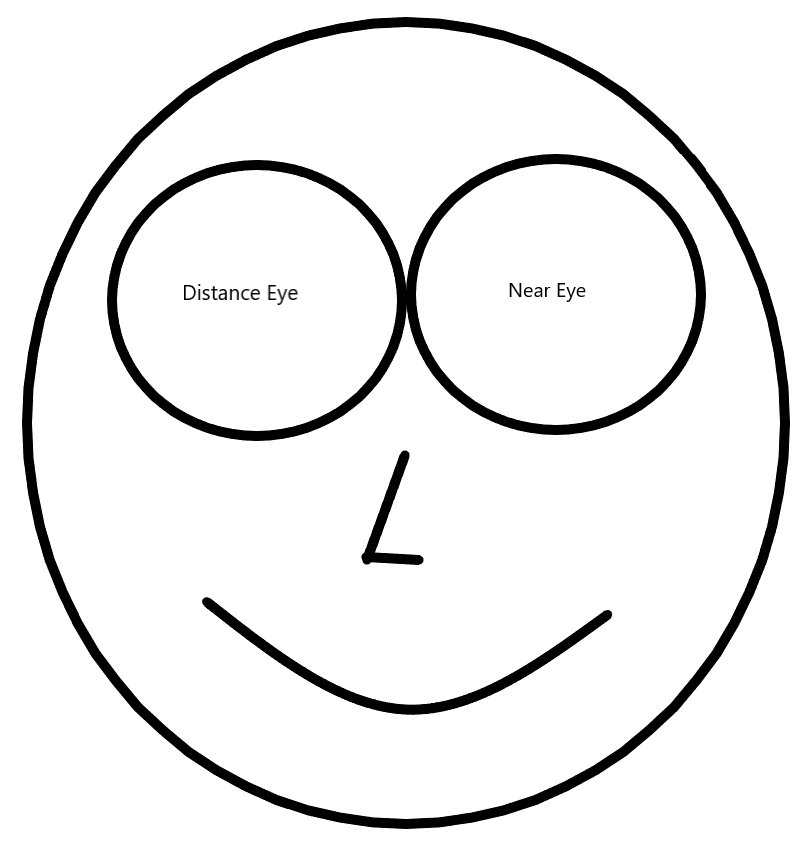
Even if a patient still sees 20/20 with their glasses, they may be eligible for refractive cataract surgery (also called clear lens exchange). This entails removing an early cataract (or even clear lens) from the eye and putting an artificial lens in its place. This is somewhat analogous to putting contact lenses or glasses inside the eye. Because of a phenomenon called presbyopia (the eye becomes stiffer with age rendering it unable to see at near without reading glasses), to be completely spectacle free following cataract surgery the patient will need to have either:
- a specialty intraocular lens placed in the eye that can focus light to both distance and near targets
- one eye targeted for distance vision while the other eye is targeted for near vision (this is called monovision)
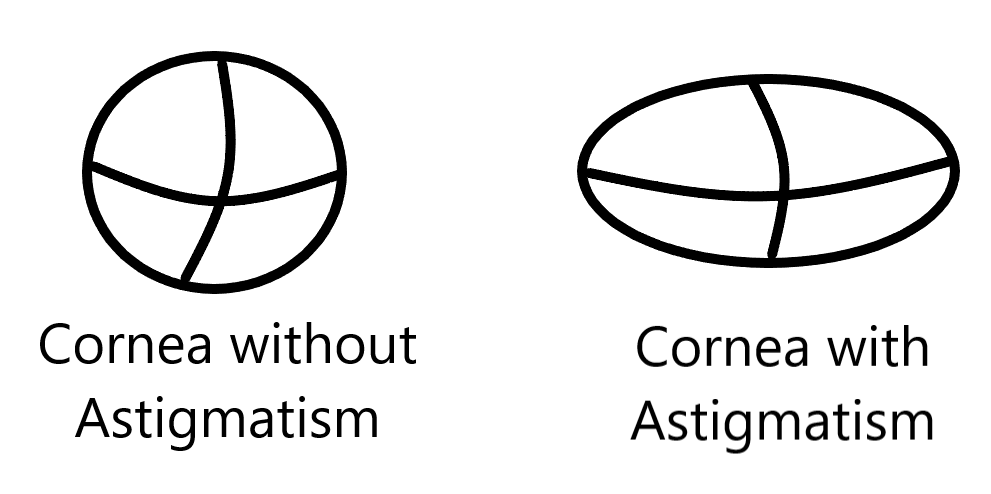
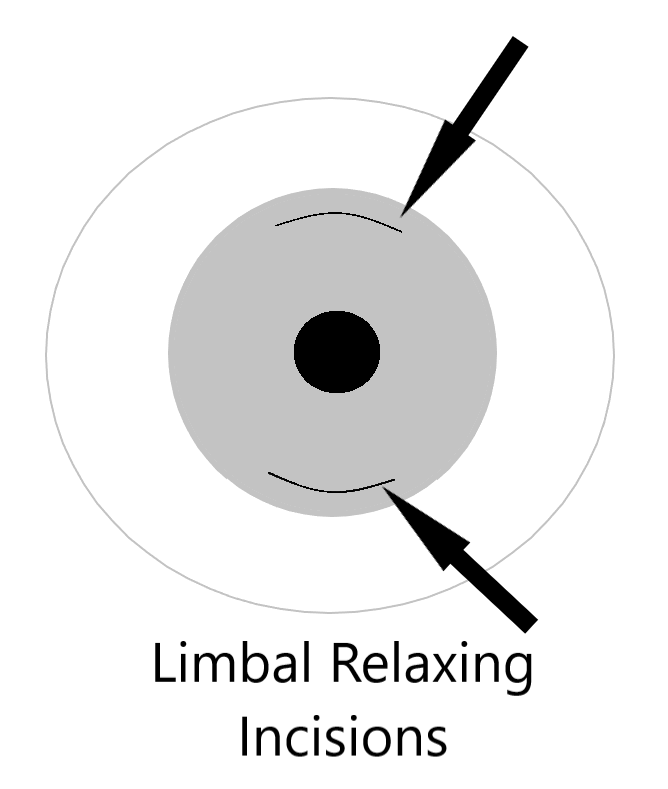
If there is corneal astigmatism (cornea is shaped more like a football than a soccer ball), the surgeon may need to place a toric lens (corrects astigmatism) or make cornea relaxing incisions to minimize post operative astigmatism.
What is presbyopia?
Presbyopia refers to the decreasing ability of the eye to focus on near objects as we age. Intraocular structures lose their elasticity over time. This is why patients in their 40s and 50s need reading glasses (and not someone in their 20s).
What is astigmatism?
Think of having no astigmatism as having an eye shaped like a soccer ball. The curvature is the same in all directions. This can be corrected with a simple lens with the same power in all directions. If the eye is shaped more like a football (one direction along the eye is steeper than another direction along the eye) then a special lens with a corresponding difference in powers along these directions is necessary to correct the vision. If corneal astigmatism is high enough, special measures will be needed to ensure minimal post surgical astigmatism.
Do I qualify for a premium lens implant?
Premium lens implant refers to toric lenses (correct astigmatism), hybrid lenses (so called extended depth of focus lenses) that give the patient distance and intermediate vision, and more traditional multifocal lenses that correct distance, intermediate and near vision. Your doctor will perform a complete eye exam, oftentimes with pictures of the retina (OCT macula) and or cornea (corneal topography) to see if you are a candidate for multifocal lenses. Multifocal lens implants divvy up light that enters the eye. They focus a portion of the light that enters the eye for distance and a portion of the light for near. Hence, less than 100% of the light passing through a multifocal lens implant is now available for distance viewing. In an eye that is struggling to see with 100% of the light already being focused for distance, this can become problematic.
- Toric Lenses: may be excluded on a case by case basis if you have irregular corneal astigmatism
- Hybrid Extended Depth of Focus lenses -> may be excluded if you have significant eye disease like advanced glaucoma or diabetic retinopathy
- Multifocal lenses -> may be excluded if you have even mild eye disease (e.g., epiretinal membrane, glaucoma, diabetes, irregular astigmatism) or a history of Lasik surgery (especially if you were far sighted prior to Lasik)
Key concept: A diseased eye (e.g., advanced glaucoma) has trouble seeing well with 100% of the light focused at distance. It will have more trouble if only 50% of the light striking the front of the eye is focused for distance.
I had Lasik or PRK laser surgery to correct my vision in the past. Will this affect my cataract surgery?
Refractive surgery like Lasik changes the curvature of the cornea as it relates to the dimensions of the rest of the eye. The cornea is flattened centrally when correcting near-sightedness while it is flattened peripherally when corrected far-sightedness. This change in curvature has the potential to cause “refractive suprise” (distance glasses are required post surgery) when the formulas used to calculate your appropriate lens power are unable to sufficiently account for this additional variable.
Note that after Lasik (especially Lasik to correct far-sightedness), patients are typically not eligible for multifocal lens implants. This may change in the future as new strategies emerge to give patients more depth of vision (e.g., lens implants that utilize a pinhole effect to increase range of vision).
Is a cornea relaxing incision or a toric intraocular lens implant a better choice to to correct my astigmatism?
This will be up to your surgeon to decide. If the surgeon is correcting more than one diopter of corneal astigmatism a toric lens implant can then be used (used for higher levels of astigmatism correction). If the corneal astigmatism is less than one diopter a relaxing incision may be used instead. There are certain levels of astigmatism where either method can be used. Talk about this with your surgeon.
Is there such a thing as cataract surgery with a laser?
There is femtosecond laser ASSISTED cataract surgery. That is to say, there a laser can perform certain steps of the surgery prior to the “manual” part of cataract surgery beginning.
- Capsulotomy -> the lens sits in a bag that your IOL implant will eventually be inserted into following cataract removal from the eye. The laser can make the circular opening for the surgeon.
- Cataract Fragmentation -> the laser can break the cataract up into small cubes that can be more easily removed from the eye by the surgeon.
- Astigmatism correction -> the laser can make cornea relaxing incisions to correct low to moderate levels of corneal astigmatism.
- Main/Side wound construction -> the laser can create self sealing access ports into the eye.
It is important to note that the surgeon still has to remove the cataract and its surrounding shell safely from the eye followed by the manual insertion of an intraocular lens implant.
Is laser assisted cataract surgery safer or better for me?
The answer to this question is evolving, especially as laser technology and algorithms continue to improve. In short, both laser assisted and “manual” cataract surgery yield excellent visual results and safety profiles.
A 2020 study in the UK showed that laser assisted cataract surgery is not inferior to manual phacoemulsification cataract surgery with respect to surgery complication rate and final vision.1
A meta-analysis looking at post 2020 data using only the latest femtosecond software did find a decreased rate of capsular rupture (i.e., breakage of the bag that holds the cataract) for laser assisted cataract surgery.2 Final visual outcomes were still the same between the two groups.
Will I be awake during cataract surgery? What kind of anesthesia is utilized?
Most commonly the patient will be awake but drowsy during cataract surgery with a combination of local anesthesia (topical numbing drops and numbing medicine injected into the eye) and intravenous sedation. For more involved procedures the doctor might perform an anesthetic injection around the eye to improve eye anesthesia and numb the eye muscles. If a patient cannot lie still while awake (e.g., severe back pain, dementia) the patient may require general anesthesia for cataract surgery.
Do I need to go to a hospital to get cataract surgery?
The majority of patients can have cataract surgery performed in an outpatient surgery center. If a patient requires general anesthesia or has other extenuating circumstances, then surgery may need to be performed in a hospital.
What are the risks associated with cataract surgery?
In general, cataract surgery is considered to be a safe surgery and is most often successful (>90% successful would be a conservative estimate). But with any surgery, complications are possible.
Complications during surgery (this list is not intended to be exhaustive, but rather to familiarize the reader with some of the more common issues that can arise in association with cataract surgery):
- Posterior capsular rupture (rupture of the bag that holds your cataract) -> this allows the jelly like substance that typically is confined to the back of your eye (vitreous) to come forward in your eye. If vitreous comes forward it is cleaned up with a procedure called a vitrectomy. The lens implant will likely have to be placed in a different location in the eye where there is adequate structural support. Estimates of posterior capsule rupture frequency vary from study to study, with 0.45% to 3.6%.3,4 If some or all of the cataract falls to the back of the eye a retina doctor may need to do a second surgery to safely remove it.
- Cataract pieces may remain in the front of the eye after cataract surgery that may require a second procedure for removal. One study found an incidence rate of 0.1%.5
- Trauma to the colored part of the eye (iris) can change its shape or color.
- Bleeding in the front of the eye (hyphema).
- Bleeding in the back of the eye (suprachoroidal hemorrhage).
Complications after surgery
- Retinal Detachment means the back layer of your eye has detached from its base. One study reported an incidence of 1.17%.6 Warning signs include flashes, floaters and vision loss.
- Infection inside the eye, also called endophthalmitis (0.013%-0.7%).7,8
- Prolonged retinal swelling that may require prolonged use of eye drop and injection treatments.
- Prolonged corneal swelling that may require prolonged use of eye drops and or a partial thickness corneal transplant.
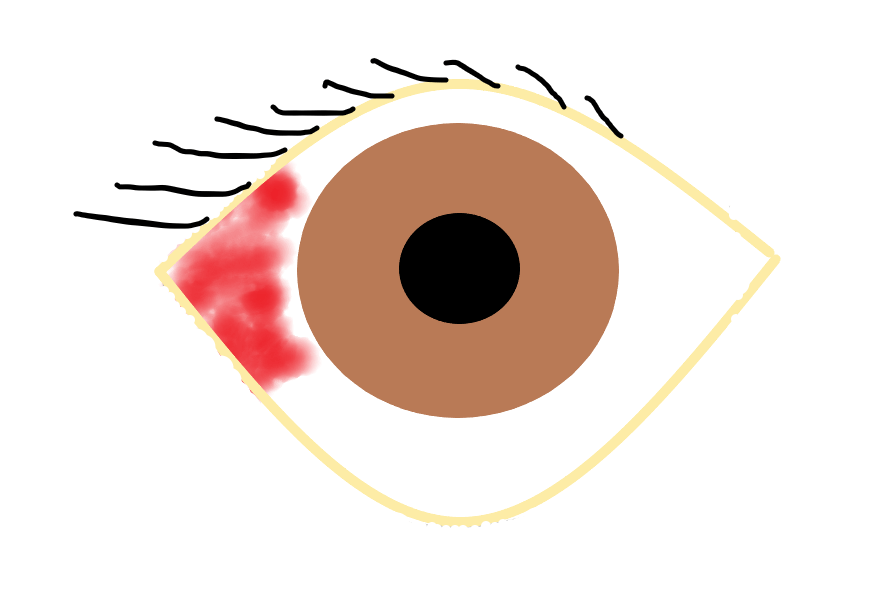
*** A part of the white part of your eye may be red following cataract surgery. If it is not associated with pain or vision loss it is most likely a subconjunctival hemorrhage. This tends to resolve on its own over 1-2 weeks. However if you have pain, worsening redness or vision loss get in touch with your health care provider to make sure this is not something more serious.
Ok so I have decided that I need to get cataract surgery? Can you summarize the main choices I have to make?
- If I have corneal astigmatism do I want to correct it (to ensure the best possible glasses free distance vision)?
- Standard monofocal intraocular lens implant (will typically need reading glasses after surgery) versus premium multifocal lens implant (may not need any glasses after surgery).
- Target both eyes for distance (standard) vs monovision (target dominant eye for distance and non-dominant eye for near vision) vs target both eyes for near (would require distance glasses post surgery).
- Laser assisted vs manual cataract surgery.
Can we do a deeper dive on each of the different intraocular lens options and strategies?
Absolutely! Click on the following button to take a deeper dive.
Disclosure: The above information is only intended for general patient education. Please direct specific questions that you may have about cataract surgery directly to your health care provider.
REFERENCES
1. Day AC, Burr JM, Bennett K et al. Femtosecond laser–assisted cataract surgery compared with phacoemulsification cataract surgery: randomized noninferiority trial with 1-year outcomes. Journal of Cataract & Refractive Surgery. October 2020 46 (10) 1360-1367 doi: 10.1097/j.jcrs.0000000000000257
2. Levitz LM, Dick HB, Scott W, Hodge C, Reich JA. The Latest Evidence with Regards to Femtosecond Laser-Assisted Cataract Surgery and Its Use Post 2020. Clin Ophthalmol. March 2021;15:1357-1363. doi: 10.2147/OPTH.S306550.
3. Chakrabarti A., Nazm N. Posterior capsular rent: prevention and management. Indian Journal of Ophthalmology . 2017;65(12):1359–1369. doi: 10.4103/ijo.ijo_1057_17
4. Vajpayee RB, Sharma N, Dada T, et al. Management of posterior capsule tears. Surv Ophthalmol. 2001;45:473–88. doi: 10.1016/s0039-6257(01)00195-3
5. Moshirfar M, Lewis AL, Ellis JH, et al. Anterior Chamber Retained Lens Fragments After Cataract Surgery: A Case Series and Narrative Review. Clin Ophthalmol. June 2021;15:2625-2633. doi: 10.2147/OPTH.S314148.
6. Javitt JC, Vitale S, Canner JK et al. National outcomes of cataract extraction. I. Retinal detachment after inpatient surgery. Ophthalmology. 1991;98:895–902. doi: 10.1016/s0161-6420(91)32204-8
7. Garg P, Roy A, Sharma S. Endophthalmitis after cataract surgery: epidemiology, risk factors, and evidence on protection. Curr Opin Ophthalmol. 2017;28(1):67–72. doi: 10.1097/ICU.0000000000000326
8. Asencio MA, Huertas M, Carranza R, et al. Impact of changes in antibiotic prophylaxis on postoperative endophthalmitis in a Spanish hospital. Ophthalmic Epidemiol. 2014;21(1):45–50. doi: 10.3109/09286586.2013.867511